Communication is linked to cognition and psychological needs, as discussed in previous blogs. Communication is about the physical ability to respond to the world around the individual. Whilst it is easy to appreciate that this is about verbal communication, it is not all that it is about.
Verbal communication is probably the most important part of this domain. So it is a question of how appropriate, accurate and reliable it is. We are all taught from a young age to say “thank you” when we are given something, “hello” when we meet someone etc. These are learned responses and as they were taught at a young age, the often are retained as memories for a long time. So if someone is asked “do you want a cup of tea” and the person answers “yes”, this does not necessarily mean they want tea, as if they are cognitively impaired, they may just be answering appropriately, but not reliably. The key issue in that circumstance is whether they drink the tea when it arrives. If they drink it about half the time, then their answer is likely to be unreliable and it is a question of pot luck if it turns out to be accurate some of the time.
Within a care environment it doesn’t matter that the person may not be able to explain complex ideas, as it is not necessarily important to the provision of their care. If they can no longer take part in a conversation about religion or politics, it won’t matter to the provision of their care. The key things the carers need to know is whether they can say that they are: hungry / thirsty / tired / hot / cold etc and very importantly – in pain. It is important that they can say this accurately, so that if for example they have had a fall, can they say they are in pain and can they say where the pain is? I have had a client who broke their hip and were not able to say they were in pain. The carers carefully checked them over and found no signs of pain and it was not until a few days later when the hip swelled that they realised there was a problem and sent them to hospital for investigation. They would not have wanted to unnecessarily send them to hospital, as it can be distressing for a cognitively impaired person to undergo the tests.
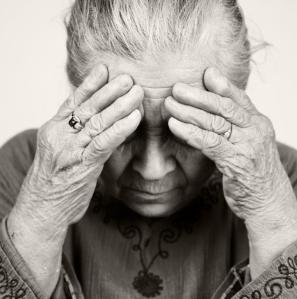
So although verbal communication is important, it is also a question about non-verbal communication, facial expression and body language. With severe dementia, eventually the individual will stop speaking, as they will forget language, but they may still be able to grimace in pain or smile etc. They may hold their arm / leg / hip / head etc to indicate that there is a pain. As time progresses, they will do less of this kind of non verbal communication as well.
There is also an aspect in this domain about familiarity with the person. This can be particularly true when the staff in a care home are stable and stay for long lengths of employment and obviously the reverse is true if the home is unsettled with the staff leaving all the time.
Accents can be difficult to understand across cultures, so if the carer and the individual do not come from the same area, this can lead to communication issues, which with familiarity may be able to overcome. This is not about non UK citizens; there are many parts of the UK that have strong accents, which will seem unfamiliar outside that area. So whether the accented person is the carer or individual, it can lead to communication issues.
This domain is also about their physical abilities, can they hear and see well, do they need a hearing aid and/or glasses? If they have a hearing aid, is it switched on? Are their glasses clean? It is not uncommon for these items to get damaged or go missing within a care home that has cognitively impaired residents. I had a client who when he was bored, would just switch off his hearing aid, if you talked to him, he would nod and then ignore you, which is linked to psychological, as it was a way that he could withdraw. I’ve seen often that if a cognitively impaired person has an issue with an “accessory”, if they stop using it for a while, they won’t return to use it, if the reason they stopped using it ends. So I’ve had clients who have stopped wearing glasses & hearing aids, but also using sticks and wearing a wig or teeth. Once the memory of using it has been lost, it seems unfamiliar when re-introduced, so is rejected. Then if the individual can’t see or hear, it will affect how they communicate.





Leave A Comment